Researchers have suggested that stabilizing airway lining mucus in aerosol infected individuals might help manage the spread of COVID-19, according to a new study published in Proceedings of the National Academy of Sciences of the United States of America (PNAS).
The findings show that while examining 194 healthy individuals, ages 19-66 years, analysts reported that exhaled aerosol particle counts varied by three orders of magnitude between individuals, with fewer than 20% of individuals exhaling 80% of total aerosol, and tended to increase with body mass index and age; aerosol production also increased with SARS-CoV-2 viral load in monkeys. This recommended that managing airway lining could decrease Coronavirus spread efficiently.
Superspreading events have distinguished the COVID-19 pandemic from the early outbreak of the disease. The studies of exhaled aerosol suggest that a critical factor in these and other transmission events is the propensity of certain individuals to exhale large numbers of small respiratory droplets. The findings of Proceedings of the National Academy of Sciences of the United States of America (PNGA) indicate that the capacity of airway lining mucus to resist breakup on breathing varies significantly between individuals, with a trend to increase with the advance of COVID-19 infection and body mass index multiplied by age (i.e., BMI-years).
Understanding the source and variance of respiratory droplet generation, and controlling it via the stabilization of airway lining mucus surfaces, may lead to effective approaches to reducing COVID-19 infection and transmission. COVID-19 transmits by droplets generated from surfaces of airway mucus during processes of respiration within hosts infected by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus. They studied respiratory droplet generation and exhalation in human and nonhuman primate subjects with and without COVID-19 infection to explore whether SARS-CoV-2 infection, and other changes in physiological state, translate into observable evolution of numbers and sizes of exhaled respiratory droplets in healthy and diseased subjects.
In their observational cohort study of the exhaled breath particles of 194 healthy human subjects and in their experimental infection study of eight nonhuman primates infected, by aerosol, with SARS-CoV-2, they found that exhaled aerosol particles vary between subjects by three orders of magnitude, with exhaled respiratory droplet number increasing with degree of COVID-19 infection and elevated BMI-years. They observed that 18 per cent of human subjects (35) accounted for 80 per cent of the exhaled bioaerosol of the group (194), reflecting a superspreader distribution of bioaerosol analogous to a classical 20:80 superspreader of infection distribution. These findings suggest that quantitative assessment and control of exhaled aerosol may be critical to slowing the airborne spread of COVID-19 in the absence of an effective and widely disseminated vaccine.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmits through the air by a combination of the large droplets exhaled when people cough or sneeze and the very small droplets people generate in their airways when they naturally breathe. How exhaled respiratory droplets vary between individuals, evolve over time within individuals, and change with the onset and progression of COVID-19 infection is poorly understood, yet critical to clarifying the nature of COVID-19 transmission--and other highly communicable airborne respiratory diseases, such as influenza and tuberculosis (TB). Generation of respiratory droplets in exhaled breath can occur by the force of the fast airflows in the upper airways that arise when we breathe, talk, cough, and sneeze. At peak inspiratory flows during normal breathing, airspeeds in the trachea and main bronchi can reach turbulent velocities.
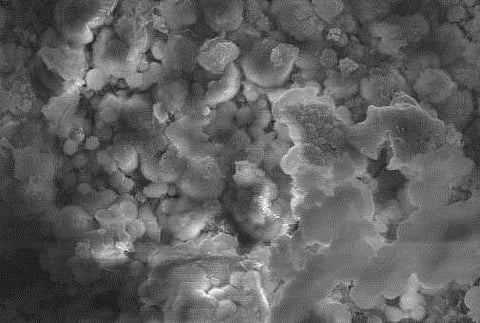
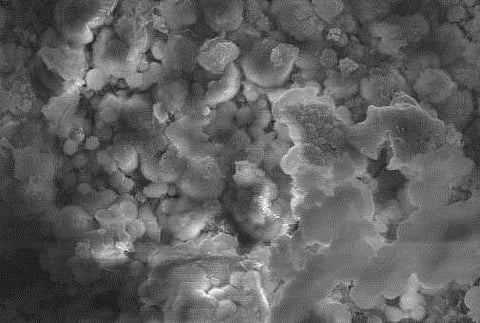
The rush of air over the thin (5 mm to 10 mm) mucus layer lining the airways can break up the mucus surface into small droplets in the way strong winds produce breakup and spray on the surface of the ocean. The nature and extent of this droplet breakup is dependent on the surface properties of the mucus itself. Among properties, most influencing droplet generation and droplet size are surface viscoelasticity (which resists the stretching of mucus surface on breakup) and surface tension (which lowers the energy expended in small droplet creation).
In airway lining mucus, both properties vary with lung surfactant type and concentration, as well as with composition and structure of mucus in close proximity to air surfaces. Surfactant and mucin compositional and structural changes, driven, in part, by physiological alterations of the human condition--including diet, ageing, and COVID-19 infection itself --may therefore be anticipated to alter droplet generation and droplet size during acts of breathing.
To ascertain whether COVID-19 infection and other phenotypical differences associated with severity of infection risk might alter airborne droplet generation from airway lining fluid during acts of breathing, they conducted two studies in human and nonhuman primates (NHPs). In our first study, we evaluated the exhaled breath of 194 human subjects at two sites to determine exhaled breath particle variations in the human population. In their second study, we measured the exhaled breath from two species of NHPs following experimental infection via inhalation of SARS-CoV-2. They then assessed exhaled breath particle evolution over the time course of exhaled aerosol particles as a function of nasal viral titer.
