I am working in an ambulatory care facility in the state of Connecticut serving multiple areas around Litchfield, Fairfield, New Haven county, Hartford county and Middlesex county (Fairfield county has the highest number of cases in the state). We also serve geographic locations that are close to Westchester county and New Rochelle where there have been unprecedented number of cases in the state of New York.
I work as a Physician assistant and my job responsibilities, especially in this circumstance are to diagnose, make clinical decisions, decide what I am going to treat my patients with, order and interpret lab tests including the COVID-19 tests, and make decisions about when to send patients to be admitted, which is usually only if they need to be intubated in this case. I perform my responsibilities by myself in the centers, with immediate access to experienced physicians over the phone.
When I was asked to serve during this crisis, my immediate reaction was that 'I must'. I took an oath over a year ago to put my best knowledge forward with the principles of medical ethics in mind -- beneficence, non-maleficence, respect for autonomy, and principle of justice, in the context of the ambiguity that is evident in almost all of medicine. However, it is the great amount of uncertainty of this novel disease we are dealing with that overwhelms me and other providers, including my classmates, and other physicians. We are still figuring out pathophysiology. There is little literature on clinical signs and symptoms, there is only hypothesis that is yet to be tested, and most of us are used to dealing with processes that we have all of the basic scientific knowledge about.
With this Coronavirus, we have so many hypotheses, that are yet to be tested and validated. We are relying so heavily on each other’s observations on the progression of the disease, the timing to make decisions on how to treat and how to progress. On a daily basis, there is a burden I feel to get it right for the best of our community, and the protection of the staff I work with. I want to make the right call, we all do, and so I pray for wisdom.
As to my personal emotion, I do think many providers would agree that emotion may be a luxury. We are just needing to do what we need to do, because the situation is alarming (some have minor cold symptoms, some can progress rapidly). Symptoms progress rapidly in some cases, and there is no cookie cutter notion, because we are seeing young and healthy patients on ventilators, although I will aggressively treat anybody with any underlying disease, smokers, will exercise caution with our first responders, and older aged folks.
At an ambulatory patient facility I am trying to treat patients and quarantine them so that we can take the burden off of our hospitals. Even with all of these efforts, I have received multiple emails in the last week requesting me to help out in the hospitals.The situation is rapidly progressing. In our neighboring state, we have had healthcare providers pass away from the disease, over 20,000 known diagnoses. Of the over 1000 cases in the state of Connecticut today, and with the first 'known' diagnosis only made on March 8, 2020, it is perhaps a euphemism to say that the situation is progressing rapidly. We also known that many are harboring the disease without knowing so, and have not been tested yet.
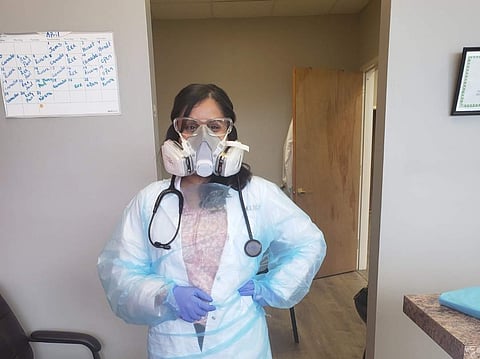
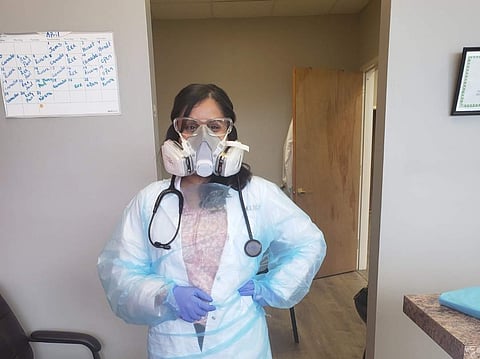
I have been blessed to have access to elastomer masks that our facilities were wise enough to preemptively acquire with filters. They are re-usable, so we are not running out of paper masks. We do experience a dearth of gowns at this time so we are re-using them, according to current Center for Disease Control guidelines. I am directly in touch, on a daily basis with providers and friends who are working in the explosive areas of New York: Queens, Bronx, and New Rochelle counties. They are exhausted for the lack of providers, exhausted for lack of PPE - any kind of mask or gown, and anxious about the uncertainty.
The United States healthcare system’s needs at this time are trained providers and protection. All physician assistants like me are trained in general medicine, no matter what specialty we have been working in, and I can certainly say that even with thousands of retired professionals who are volunteering (nurses, doctors, etc), there is still a need. There is concern that we will run out of intensive care facilities here in Connecticut. Although most cases are mild, the sheer large volume of people who are becoming infected, makes the proportion of those needing emergent/ intensive care large too.
Healthcare providers in addition to the above, are actually developing anxiety, depression, and are unrested because of overwhelming cases. We need the public to help us out by staying at home and limiting social contact, because there will be exponential number of cases once a threshold is reached. Even at home, anyone who has the sniffles/ cough/ shortness of breath, should be put in a separate room with separate access to bathroom. Keep older parents, and those with diabetes, hypertension, asthma, or other respiratory conditions, separate from those of you who are going out to work. Stay at home.
My hope is in my faith in times of uncertainty. To those of you at home in India, I behoove you to be concerned for your fellow Indian, by maintaining hygiene as much as possible, and being considerate that just because you many not have symptoms, you can pass on COVID-19 to someone who can die from it. You are your brother’s keeper.
(As told to Blessy Mathew Prasad)
